Phoebe Chastain
MPH, Public Health Administration & Policy
Advisor:
Katy Backes Kozhimannil
Keywords:
Rural telemedicine
Abstract
Background:
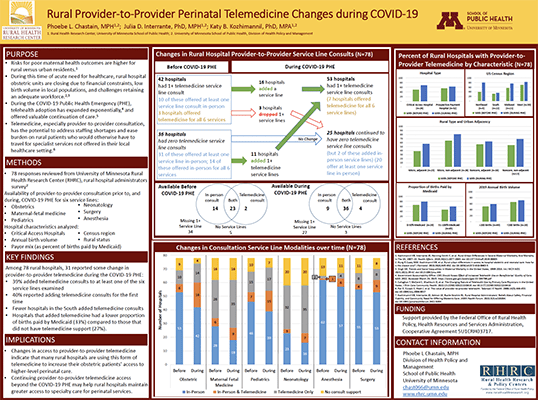
Workforce challenges, including adequate staffing and skill level, in rural hospitals with low birth volume can make providing safe maternity care challenging. Telemedicine, especially provider-to-provider consultation, has the potential to address staffing shortages and ease burden on rural patients who have to travel for specialist services unavailable at their local hospital. Little is known about the variation in addressing workforce shortages through provider-to-provider telemedicine in rural obstetric settings.
Objective:
To describe how provider-to-provider telemedicine among rural hospital-based maternity care clinicians changed before and during the COVID-19 public health emergency (PHE).
Methodology:
The Rural Health Research Center (RHRC) conducted a survey of rural hospital clinicians and administrators across the U.S. about their experiences providing obstetric care. I analyzed responses from 78 rural hospital administrators to questions related to availability of telemedicine supports for obstetric clinicians through provider-to-provider consultation for six service lines (obstetric consultations, maternal-fetal medicine, pediatrics, neonatology, anesthesiology, and surgery) prior to March 2020 and during the COVID-19 PHE (March 2020 to July 2021).
Results:
Among the 78 respondents, 42 (54%) hospitals reported having at least one service line available through provider-to-provider telemedicine at the start of the study period. The most common service line was neonatology (n=36) followed by maternal-fetal monitoring (n=34). Thirty-one hospitals reported some change in telemedicine supports during the COVID-19 PHE (39% added telemedicine support to at least one service line), and 40% of these reported adding telemedicine supports for the first time (n=11). Hospitals that increased telemedicine offerings added support most commonly for obstetric consultations (60%) and maternal-fetal medicine (40%). Hospitals that added telemedicine had a greater proportion of births paid by private insurance (33.3%) compared to those that did not add telemedicine support (26.7%) and had a greater number of annual births (average of 527 births in 2019 versus 312).
Conclusions:
Changes in access to provider-to-provider telemedicine during COVID-19 indicate that many rural hospitals are using this form of telemedicine to increase their obstetric patients’ access to higher-level care. Extending policy options to support provider-provider telemedicine beyond the COVID-19 public health emergency may help rural hospitals maintain greater access to specialty care for obstetric patients.
View Poster (PDF)
