Casey Rieck
MPH, Public Health Administration & Policy
Co-Authors:
Katie White, Melissa Buescher
Advisor:
Dr. Katie White
Educational Objectives:
Evaluate nursing adherence to device use using the RE-AIM framework. / Analyze the proportion of air bubbles in central venous lines before and after device implementation.
Keywords:
Implementation Science, Pediatrics
Abstract
Objective: Central venous lines (CVLs) are necessary to manage critically ill pediatric patients, but inadvertent air bubbles in these lines can lead to an air embolus within pulmonary circulation. Such air emboli may have a larger impact on children with congenital heart disease than patients with normal physiologic conditions. This study sought to decrease the proportion of CVLs that contain air bubbles in a pediatric cardiac intensive care unit (CVICU) through a quality improvement initiative.
Design: An interrupted time series design was performed with the introduction of two devices to eliminate such air bubbles: an anti-siphon value (ASV) was first introduced in April 2016 followed by the addition of the neutron cap a year later. Nursing adherence was assessed using the RE-AIM implementation framework.
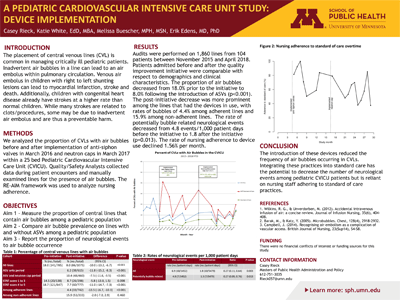
Measurements and Main Results: Audits were performed on 1,860 lines from 104 patients between November 2015 and April 2018. Patients admitted before and after the quality improvement initiative were comparable with respect to demographics and clinical characteristics. The proportion of air bubbles decreased from 18.0% prior to the initiative to 8.0% following the introduction of ASVs (p<0.001). The post-initiative decrease was more prominent among the lines that actually had the devices in use, with rates of bubbles of 4.4% among adherent lines and 15.9% among non-adherent lines. The rate of potentially bubble related neurological events decreased from 4.8 events/1,000 patient days before the initiative to 1.8 after the initiative (p=0.013). The rate of nursing adherence to device use declined 1.56% per month.
Conclusions: The introduction of these devices reduced the frequency of air bubbles occurring in CVLs. Integrating these practices into standard care has the potential to decrease the number of neurological events among pediatric CVICU patients but is reliant on nursing staff adhering to standard of care practices.
View Poster (PDF)
