Lorna Bittencourt
PhD, Environmental Health
Co-Authors:
Dana Rubenstein, Devon Noonan, F Joseph McClernon, Dana Mowls Carroll
Advisor:
Dana Mowls Carroll
Keywords:
Smoking, Disparities
Abstract
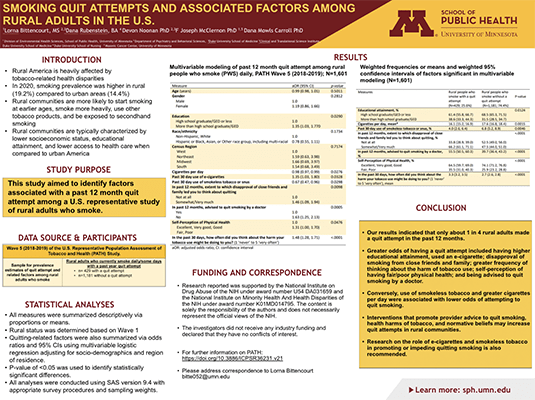
Introduction: Rural American communities are heavily affected by tobacco-related health disparities. Identifying factors associated with smoking cessation success among rural adults is necessary for the development of effective public health efforts. This study aims to evaluate the prevalence of quit attempts and factors that promote or impede quit attempts among rural adults who smoke daily.
Methods: We analyzed data from Wave 5 (2018 to 2019) of the Population Assessment of Tobacco and Health (PATH) study, a U.S. nationally representative prospective cohort study. We conducted weighted, multivariable logistic regression to identify factors, encompassing socio-demographics, tobacco use behaviors, normative beliefs, and perceived health and health care interactions, associated with attempt to quit smoking in the past 12 months among rural adults who smoke. Backward selection was used to identify variables included in the final model with statistical significance set at p<0.05.
Results: Among 1,610 rural adults who smoked daily, the prevalence of a quit attempt in the past 12 months was 25.6% (95% CI: 23.2, 28.2). In multivariable modeling, factors associated with greater odds of a quit attempt included: having more than high school/GED education (aOR = 1.35, 95% CI: 1.03, 1.80), past 30 days use of an e-cigarette (aOR=0.98 95% CI: 0.97-0.99), disapproval of smoking from close friends and family (aOR= 1.46, 95% CI: 1.09-1.94), greater frequency of thinking about the harm of tobacco use (aOR = 1.48, 95% CI: 1.28, 1.71), fair/poor physical health (aOR=1.31, 95% CI: 1.00, 1.70) and being advised to quit smoking by a doctor (aOR =1.63 , 95% CI:1.25, 2.13); whereas, past 30-day use of smokeless tobacco (aOR = 0.67, 95% CI: 0.47, 0.96) and greater use of cigarettes per day (aOR = 0.67, 95% CI: 0.47, 0.96) were associated with lower odds of a quit attempt.
Conclusion: Only 1 in 4 rural adults who smoke made a past year quit attempt. Based on these findings, interventions that promote provider advice to quit smoking, health harms of tobacco, and normative beliefs may increase quit attempts in rural communities. Research on the role of e-cigarettes and smokeless tobacco in promoting or impeding quitting smoking is also recommended.
Support
This study was supported by the National Institute on Drug Abuse of the NIH under award number U54 DA031659 and the National Institute On Minority Health And Health Disparities of the NIH under award number K01MD014795.
View Poster (PDF)
